Heart Failure
What is heart failure?
Heart failure occurs when the heart becomes less effective at pumping blood around the body.
Heart failure does not mean your heart function has completely failed. Instead, it means that your heart is failing to work as well as it should. Many people with heart failure have a good quality of life. Lifestyle changes, medications, and other therapies can help your heart work better.
What Happens in Heart Failure?
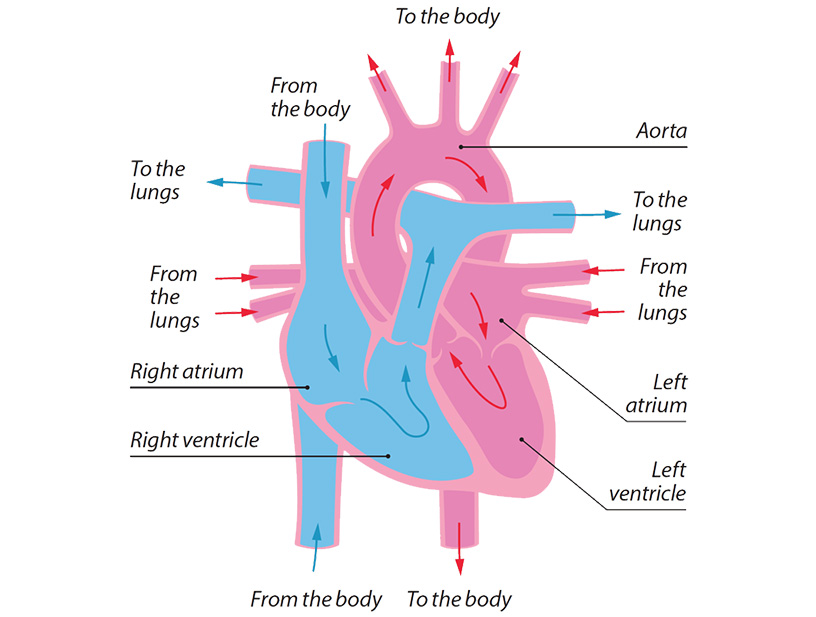
The ventricles are the heart’s main pumping chambers. They contract then relax with each heartbeat. Each contraction pushes blood out into the lungs and the body. During relaxation, the ventricles refill with blood in preparation for the next heartbeat.
How the heart works:
The left ventricle is the strongest and most important chamber of the heart. It collects oxygen-rich blood from the lungs and pumps this to the rest of the body. When its pump function is compromised, symptoms of fatigue, breathlessness, and fluid retention occur.
Why is my heart’s ejection fraction (EF) important?
The ejection fraction (EF) measures the strength of the left ventricle and helps determine how well your heart is pumping. It refers to the percentage of blood that is ejected from the left ventricle with each contraction.
EF can be measured by imaging the heart with echo, CT, MRI, or nuclear scanning. A low EF is one sign of heart failure and indicates that the strength of the heart muscle is compromised.
- > 50% – The strength of the main pumping chamber is normal
- 35 – 50% – The strength of the main pumping chamber is below normal
- < 35% – The strength of the main pumping chamber is low
Heart failure can also occur with a normal or preserved EF. In this case the main problem is that the heart muscle is stiff and fails to relax properly even though it can contract at full strength. This prevents the heart from filling efficiently before each heartbeat. One clue that this is occurring is enlargement of the left atrium due to back pressure.
Types of heart failure
- Heart failure with reduced EF (HFREF) – Inadequate heart muscle strength
- Heart failure with preserved EF (HFPEF) – Inadequate heart muscle relaxation
Why do I have heart failure?
There are many reasons why heart failure occurs.
The most common are:
- Heart attack
- High blood pressure (hypertension)
- Heart valve disease
- Cardiomyopathies (diseases of the heart muscle)
Other important causes include
- Arrhythmias such as AF and atrial flutter
- Alcohol and recreational drugs
- Viral infections of the heart
- Thyroid hormone excess
- Some forms of chemotherapy
There are other causes of heart failure, and in some cases the cause is unknown.
What are the symptoms of heart failure?
Heart failure may result in minimal symptoms that are barely noticeable to severe symptoms that interfere with daily life.
The key symptoms include:
- Breathlessness. This may be with activity or at rest.
- Swelling. You may notice swollen feet, ankles, legs, or abdomen.
- Fatigue. You may feel unusually tired and unable to perform physical activity.
Heart failure can be described as acute or chronic:
- Acute heart failure is when the symptoms of heart failure come on suddenly. If this happens, you will probably need to be treated in hospital. Your doctor may tell you that you have ‘acute heart failure’ either if you are diagnosed with heart failure for the first time, or if you have long-term (chronic) heart failure and your symptoms have suddenly become worse.
- Chronic heart failure is when someone has long-term symptoms of heart failure.
What causes heart failure symptoms?
Heart failure happens because your heart is not pumping as well as it should. This can cause a number of problems. It can lead to a build-up of fluid that backs up into the lungs. This fluid congestion causes breathlessness. Sometimes doctors refer to it as ‘congestive heart failure’.
Also, because blood is not pumped to the kidneys properly, the kidneys can retain salt and water. This extra fluid in your body can cause swelling in your ankles, feet or legs, or in the small of your back, abdomen or groin. The extra fluid can also cause sudden weight gain.
Heart failure can also cause fatigue because your heart may not be able to deliver enough blood and oxygen to the muscles in your body.
Breathlessness and swollen ankles are not always caused by heart failure. These symptoms can also be caused by other conditions. For example, breathlessness can be caused by lung problems, and swollen ankles can be caused by having surgery or being very overweight.
What is the relationship between arrhythmias and heart failure?
Certain arrhythmias, such as atrial fibrillation, have a close relationship with heart failure. Sustained arrhythmias that are rapid or irregular can cause heart failure. Conversely, heart failure produces electrical instability of the heart and may result in arrhythmias.
The following arrhythmias may cause heart failure:
- Atrial fibrillation
- Atrial flutter
- Ventricular arrhythmias
- Any incessant (non-stop) rapid arrhythmia
Heart failure is an important cause of the following arrhythmias:
- Atrial fibrillation
- Ventricular tachycardia
- Ventricular fibrillation
What tests do I require for heart failure?
You may require the following initial tests:
- Blood Tests – To determine the severity of your heart failure and see if there is an underlying condition contributing to your heart failure
- ECG – To evaluate your heart rhythm
- Holter Monitor – To evaluate your heart rhythm over a 24 hour period for arrhythmia
- Echocardiogram – To evaluate the structure and function of your heart, and to measure your heart’s ejection fraction (EF), normally >50%
Learn more about the different Heart Tests here.
Can heart failure be cured?
Unfortunately, heart failure can’t be cured yet. But with ongoing treatment and management of your symptoms and lifestyle, many people can lead a full and good-quality life.
Your treatment has the following aims:
- To improve your symptoms
- To allow you get on with your usual activities
- To prevent deterioration of your condition
- To prolong your lifespan
It may be possible to treat some of the conditions that can cause heart failure, such as arrhythmias, thyroid problems, and heart valve disease. Treating the cause can improve your symptoms and quality of life, but it is unlikely that your heart will make a complete return to its prior healthy state.
Heart failure itself is managed with simple lifestyle measures, a combination of medications, and in some cases other more specialised therapies.
Can heart failure worsen?
In some individuals, heart failure does get worse with time. Making changes to your lifestyle, taking your medicines, and controlling your symptoms and can all help to keep you as well as possible.
Treatments are constantly being improved and new ones are becoming available. Our clinic has a special interest in this area. If you would like to be involved in research we are conducting, please do let our staff know.
Does heart failure shorten my lifespan?
It is not possible to tell anyone with heart failure how long they might live. Heart failure affects different people in different ways. It does shorten the lives of some people, but others live with heart failure for many years. Your outlook will depend on the cause of your heart failure, your age, your symptoms and your general health.
How is heart failure treated?
Simple measures can help manage symptoms:
- Weigh yourself regularly. Heart failure can cause fluid retention, sometimes many litres if left unchecked. Weighing yourself regularly is one way to monitor this.
- Limit your salt intake to 2,000 mg a day. This helps maintain your blood pressure in the normal range and helps prevent fluid retention that results in swelling and breathlessness.
- Exercise regularly to strengthen your heart. All it takes is 30 minutes a day of activity, even if that activity is walking. Talk to your GP about an exercise program that is right for you.
- Fluid medications called diuretics are sometimes necessary to help rid the body of excess fluid by increasing urine output. Frusemide is a commonly used option.
Medications to strengthen the heart and prevent deterioration
- If you have heart failure with reduced EF, there are medications that can prevent deterioration of heart function, and improve the overall strength of your heart.
- Two key medications include ACE-inhibitors and beta-blockers.
- Other medications are also useful in certain situations and for certain forms of heart failure and we will discuss these with you if relevant.
Learn more about heart failure medications here.
Cardiac Resynchronization Therapy (CRT)
- Heart failure sometimes occurs when the heart’s main pumping chamber, the left ventricle, is not only weakened but pumps in an uncoordinated fashion.
- This unsynchronized pumping action results in the heart wobbling rather than squeezing with each heartbeat.
- Some individuals may benefit from implantation of a special type of pacemaker called a “biventricular pacemaker” that helps resynchronize the heart’s pumping action.
Defibrillator (ICD) Implantation
- Some individuals have an increased risk of dangerous arrhythmias arising from the lower chambers. These arrhythmias are termed ventricular tachycardia (VT) and ventricular fibrillation (VF).
- The danger of these arrhythmias is that they may lead to cardiac arrest and sudden death. Often, only an immediate electric shock to the heart will correct these abnormal rhythms.
- Medications significantly reduce the risk of VT and VF. However, certain individuals with ongoing risk may benefit from implantation of a cardiac device called a defibrillator which monitors the heart’s rhythm constantly and delivers a lifesaving shock if necessary.
- ICDs can function as pacemakers, therefore you would need only one device if you also required a pacemaker. A biventricular pacemaker can also be incorporated into an ICD and this is called a biventricular ICD.
- Your doctor will advise you regarding which device suits your condition best.
Learn more about ICD implantation here.
Cardiac Transplantation
If you have severe heart disease and your symptoms cannot be controlled with other treatments, you may be referred for assessment for a heart transplant.