Pacemaker Implantation
What is a Pacemaker?
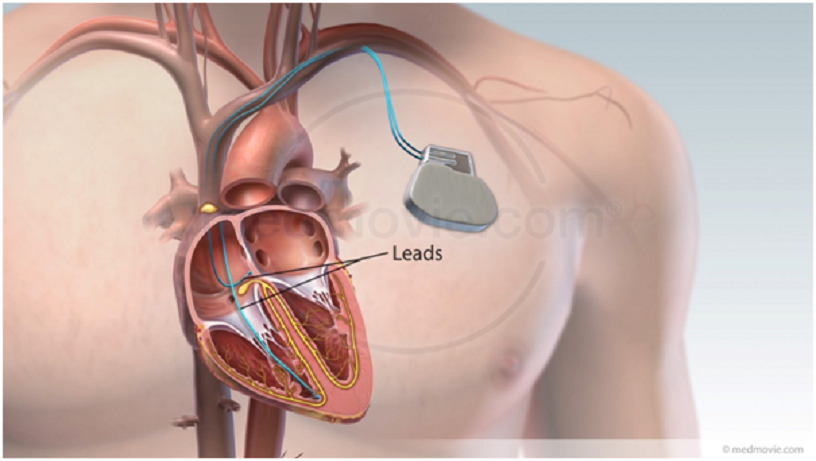
A permanent pacemaker (PPM) is small device that serves as a backup electrical system for your heart. It is implanted beneath the skin and below the collarbone, with one or two leads positioned within the heart.
Your heartbeat is regulated by an electrical system.Every normal heartbeat starts with an electrical impulse generated by the heart’s natural pacemaker, the sinus node. This impulse first spreads through the upper chambers, then is carried to the lower chambers via special electrical cables.
If any part of this natural electrical system becomes faulty, then the heart may beat too slowly or may stop momentarily. This is called bradycardia, and resulting in fatigue, dizzy spells and blackouts.
An implantable pacemaker detects bradycardia, and sends electrical impulses to your heart through its electrical leads to stimulate the upper or lower chambers to contract so that it beats at a normal heart rate.
Preparation
Pacemaker implantation may be performed during an elective admission, or during an unplanned inpatient stay.
If you are having an elective procedure, you will receive a letter from the hospital bookings clerk or doctor’s secretary outlining the date, time, and other details of your hospital admission for the procedure. A nurse may call you to confirm your personal and medical details.You will need to attend a blood collection service for a blood test within the week prior to your procedure.
You will receive specific instructions about any medications changes that are necessary prior to your procedure. If you are unsure about the instructions, please do contact the clinic for clarification.
You must fast for at least six hours before your procedure. If your procedure is in the morning or early afternoon, do not eat or drink after midnight, except for a sip of water to help you swallow your pills.If your procedure is in the mid to late afternoon, you may have a light, early breakfast.
Admission
During your admission, pre-operative checks will be performed before transfer to the operating room. The operating room has a movable patient bed, an X-ray machine, ECG monitors, and other equipment.
ECG electrodes and patches will be attached to your chest and back. These will feel cool on your skin. An anaesthetist will insert a fine intravenous tube usually into the back of your hand before administering a sedative. A second tube may be placed into the artery of your wrist to monitor blood pressure. The entire procedure takes 1 h and is normally performed under local anaesthesia with sedation to make you comfortable.
Procedure
The pacemaker is implanted beneath the skin, usually below the left collarbone. The area is cleaned with a sterile solution. You will be given an antibiotic for protection against microbes and a sedative through an intravenous line. A large sterile sheet will cover your body and will partially cover your face.
You will receive a local anaesthetic injection to the area below the collarbone which will sting momentarily. Thereafter, the area will be numb. You may feel some pressure in the area as the doctor is working, and you should feel no pain. If you do, please inform anaesthetist or nurse who will be by your side attending.
One or two leads will be threaded through a vein and positioned in your heart under X-ray guidance. These are then connected to the pacemaker which is positioned under the skin before the incision is sewn over and dressed.
Risks
Pacemaker implantation is a routine procedure. Some bruising can occur and is normal. More serious complications are uncommon, and are dealt with promptly where they arise.
These include the following.
- Infection. Infection at the surgical site is treated with antibiotics. The pacemaker may need to be removed to clear the infection.
- Haematoma. This is a large blood clot beneath the skin that causes swelling and may take some weeks to settle.
- Pneumothorax.Partial collapse of the lung may due to a small perforation from a needle. This often heals spontaneously although in some cases a small tube to the chest is required to help drain the air leak. This delays discharge by a few days.
- Lead dislodgement. A pacemaker lead sometimes moves out of place shortly after the procedure, and needs to be repositioned.
- Cardiac perforation. This is a rare complication where one of the pacemaker leads penetrates the heart wall causing blood to accumulate around the heart. If this occurs, it will be dealt with immediately.
Recovery
After the procedure, you will return to the recovery ward before being transferred to a normal hospital ward.
It is usual to stay in hospital for 1-2 nights after the procedure. There will be some bruising and discomfort at the implant site which normally settles over the following weeks.
You will need to arrange for a family member or friend to pick you up from the hospital following discharge. A follow-up appointment will be arranged 1 month post procedure or earlier if necessary.
Discharge Information
- Wound care. A waterproof dressing is placed over your incision and must remain in place for a week. You may remove it carefully thereafter. Make an appointment to see your GP a week after the procedure to check that the wound is healing well. You may have your GP remove the dressing if you prefer.
- Rest and recovery. For 4 weeks, you must avoid strenuous exercise, heavy lifting, and raising your elbow above your shoulder. This includes golf, bowling, and swimming. You may return to driving after 2 weeks, unless you are disqualified from driving for another reason.
- Contact details. Prior to your first follow-up appointment, it is best to contact the treating team for any post-procedure issues, as they will be most familiar with the details of the procedure. For public patients, contact the Alfred Heart Centre on 03 9076 3263. For private patients, contact the Heart Rhythm Clinic on 03 8560 0535. If the clinic is closed or the treating doctor or nurse not available, please proceed to your GP or local emergency service for evaluation.
Living with a Pacemaker
- Your pacemaker will need to be checked around 1 month after implant.
- Thereafter, you will need to have it checked every 3 to 6 months.
- When the battery runs low, you will need surgery to replace the pacemaker.
- Tell your doctors and dentist that you have a pacemaker. Certain types of medical equipment may affect the way the pacemaker works.
- Tell airport security that you have a pacemaker.
- Carry an ID to let others know that you have a pacemaker.
- Household microwaves, electric appliances, most office and light shop equipment will NOT affect your pacemaker.
- If you work around industrial microwaves, electricity, or large motors, ask your doctor about possible effects.
Microwaves and Mobile Phones
Microwave ovens, electric blankets, remote controls for TV and other common household appliances won’t affect your pacemaker.
You can use a cell phone, too, if you take these steps:
- Hold the phone to the ear on the side of your body opposite from your pacemaker.
- When your phone is on, keep it at around six inches away from your pacemaker. For example, don’t carry your phone in your breast pocket over your pacemaker.